posted 23rd August 2022
Pelvic pain can have a variety of etiologies. Some common gynaecological reasons of pelvic discomfort include endometriosis, adenomatous polyps, ovarian cysts, pelvic congestion, pelvic inflammation, and adhesions. About one-third of patients do not have a specific gynaecologic explanation for their discomfort and it could be from other organs like the bowel.
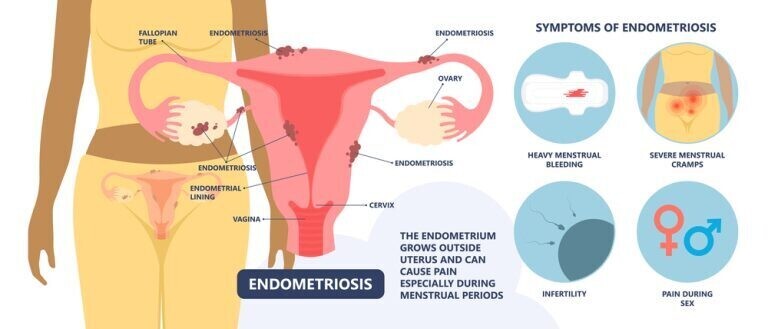
Endometriosis
It is not uncommon for the endometrial tissue (the endometrium) to appear outside the uterus, most commonly in the ovaries and fallopian tubes, the lining of the abdomen (the peritoneum), the colon, or the bladder. This condition is known as endometriosis. Hormones have the same effect on these tissues as they do on the uterine lining.
During menstruation, these tissues become inflamed and bleed, leading to scarring of surrounding organs like the bowel, ureters and fallopian tubes. In most cases, hormonal contraceptives can be used to treat the symptoms. Surgery is offered in specific situations for example if you have severe symptoms that are not responding to medical treamtment, Large cysts causing symptoms, fertility problems or involvement of any vital organs like bowel or ureters.
Around two million British women are thought to be affected by the disease, diagnosed between the ages of 25 and 40. Menopausal women are less likely than other women to develop endometriosis.
Symptoms of endometriosis
Chronic pelvic pain
Chronic pelvic pain is the most common symptom.
Period pains
This is a common problem and, on its own, is unlikely to be related to Endometriosis. Period pains can be exacerbated in Endometriosis due to increased inflammation. Other conditions like Adenomyosis cause more period pains, and this often coexists with Endometriosis.
Deep pain during intercourse
This is also a common problem in patients with severe Endometriosis. Common reasons are the presence of Endometriosis in the vagina (rectovaginal Endometriosis), large endometriotic cysts of the ovaries, or other conditions like Adenomyosis.
Painful bowel movements
Patients with severe Endometriosis often have painful bowel movements. This is more often seen during periods but can also happen on a regular basis. The most common reason is that the bowel (Rectum) is tethered to the vagina by Endometriosis. There is often an endometriotic nodule in the area between the vagina and rectum. Sometimes this can also be caused by endometriotic cysts that press on the bowel.
Shooting pain in the rectum
This is another commonly reported symptom and one of the classical descriptions given by many patients with rectovaginal Endometriosis. This is due to the presence of Endometriosis involving the uterosacral ligament and the rectovaginal area.
Pain radiating to the Back
This is often seen when Endometriosis involves the uterosacral ligaments.
Pain radiating to thighs
This is often seen when Endometriosis involves the ovaries where the ovaries are stuck to the side of the pelvis. This causes irritation of the nerves supplying the thigh, leading to this pain.
Bleeding per rectum
This is a common problem not always related to Endometriosis. Due to Endometriosis, bleeding from the rectum is seen during periods and therefore has a cyclical pattern. It is usually dark period type blood as opposed to fresh blood seen in other causes like piles or fissures.
Urinary Symptoms
When Endometriosis has affected the bladder, patients can experience symptoms like bladder pain and urgency. Rarely if the Endometriosis has infiltrated the bladder wall- there could be blood in the urine during periods.
Causes of Endometriosis
The reasons for endometriosis aren’t fully known. However, there are various theories. One such notion is that such cells were present in these locations throughout the formation of pelvic organs. Another theory is related to retrograde menstruation.
What is the best way to diagnose deep Endometriosis?
A combination of clinical evaluation, imaging and laparoscopy is the best way to diagnose Endometriosis.
Although laparoscopy is considered the gold standard, in my opinion, this should be used as a complementary diagnostic tool to basic clinical evaluation (symptoms and clinical examination) by an Endometriosis specialist.. While superficial Endometriosis is easier to see on laparoscopy, there is rarely the cause of acute or chronic pelvic pain. Pelvic pain is usually caused by deep infiltrating Endometriosis. In rare instances, if the Endometriosis is in deeper tissues, this may not be seen on laparoscopy.
What type of imaging is best for Endometriosis – is it Ultrasound or MRI?
Ultrasound ( USS) is an excellent tool to diagnose rectovaginal Endometriosis, provided it is done by a specialist with experience in endometriosis scans. USS is therefore very much dependent on the skill and expertise of the person doing the scan. This is not widely available.
MRI, on the other hand, is less operator dependent but needs to be interpreted by radiologists with experience in Endometriosis. It also gives a broader view of the pelvis, which cannot be obtained by USS.
Types of Endometriosis
Mild, moderate, and severe are a few of the numerous levels of severity. Deep and superficial is another one. There are also different stages of endometriosis with stage 4 being the worst. When discussing a patient’s condition, doctors frequently combine the two terms. When it comes to endometriosis, the more severe the condition, the more serious it is deemed.
Medical Treatment
This is usually with painkillers and hormone medications. Medical treatment or a conservative approach is suitable for women where symptoms are mild and examination/ scans are normal. In severe endometriosis usual medical treatments are unlikely to work.
GnRH analogues- This includes injections like Zoladex or Prostap and Nasal spray called Synarel. These are used to suppress the endometriotic lesions. This is very effective in controlling symptoms of endometriosis and also in regressing the lesions. This is usually given for 6-12 months to help with symptoms prior to surgery.
Laparoscopic Surgery
This is usually reserved for patients with severe disease on clinical examination, fertility issues or based on symptoms/ scans. Excision of endometriosis is the preferred option but in superficial disease cauterization can also be done. In patients with severe disease a more complex surgery may be required. This might involve taking bowel prep before surgery in some patients. To avoid recurrence after surgery, hormonal therapy is frequently suggested unless you are trying for pregnancy. A two-stage operation may be necessary in some patients with severe illnesses.
Centres for Endometriosis
The British Society of Gynaecological endoscopists ( BSGE) has selected specialist centres within the UK to provide treatment for severe endometriosis. Such centres are assessed on an annual basis. These centres perform more complicated procedures that involve other specialities like urologists, colorectal surgeons and pain specialists. Dartford and Gravesham NHS Trust is such a BSGE approved endometriosis tertiary centre where Mr Kovoor is the lead for this service.
Endometriosis and Pregnancy
Endometriosis is a common cause of infertility in women. There is evidence to suggest that laparoscopic treatment of endometriosis helps with fertility.
Other Common Causes of Pelvic Pain
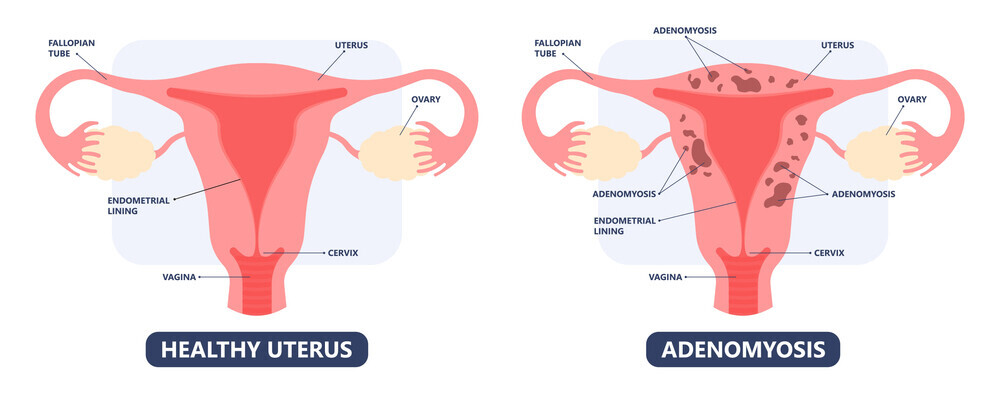
When the uterine lining (the endometrium) enters through the uterus’s muscle wall (the myometrium), it is known as Adenomyosis. These endometrial cells grow over time, resulting in swelling, discomfort, and abnormal bleeding. In simple terms adenomyosis is actually endometriosis of the uterine wall. The symptoms from adenomyosis can be very debilitating.
What are the symptoms of Adenomyosis?
One of the most prevalent symptoms of this condition is painful periods and pain in the intervals between periods (often known as the “phantom period”), heavy or irregular periods, and pain or discomfort during sexual activity are also the symptoms of Adenomyosis.
Who is prone to getting Adenomyosis?
Middle-aged women and women who have given birth are more likely to be diagnosed with it. Adenomyosis is more common in women who have given birth via caesarean section. It is not Adenomyosis often coexists with other disorders such as Endometriosis of the pelvis, fibroids, and PCOS.
How is Adenomyosis diagnosed?
A pelvic examination is helpful as it often shows an enlarged and tender uterus. Useful imaging modalities include ultrasound and MRI scans.
How is Adenomyosis managed?
Patients are treated according to symptoms. Anti-inflammatory drugs like mefenamic acid and neurofen can be administered to treat mild symptoms. It’s best to take this a few days before your menstruation begins. It can help alleviate the pain associated with menstruation by reducing the inflammation. Additionally, Tranexamic acid can be taken to prevent excessive bleeding during this time.
Hormone Therapy
Contraceptive pills, injections, and IUS are all choices available. Patients react differently to each of these, it’s a trial and error method to find the most suitable option. Uterine artery emobolisation for treatment, I have not had much success with this method. In embolisation, tiny particles are utilised to block the blood supply to the uterus. This is performed by interventional radiologists.
Surgical Intervention
Localised excision may be possible if the lesion is small but recurrence rates are high.
Hysterectomy
This is the only treatment that has excellent results. A laparoscopic or vaginal (V NOTE) procedure can be used.
Is endometrial ablation an option?
Endometrial ablation exacerbates adenomyosis-related pelvic pain, in my opinion. Patients typically require hysterectomy as a result of the terrible aches they experience after the procedure, despite the fact that it may help with their periods.
Does Adenomyosis Cause Infertility?
Adenomyosis has been linked to infertility.
Caesarean Section scar niche
This is a defect in the C section scar. There are several causes for developing a scar niche. Some of these are a tilted womb, full dilatation c section, post op infection and multiple c sections
Following are some of the symptoms reported by patients with scar niches
- Chronic Pelvic pain.
- Postmenstrual spotting.
- Postcoital bleeding.
- Difficulty in conceiving
How is Scar Niche diagnosed?
- Ultrasound scans
- Saline sonography
- MRI scans
- Hysteroscopy
What are the treatment options for the Scar Niche?
There are a number of medical options to consider. Stopping or reducing the flow of blood is the primary objective. Contraceptive injections and pills can also be used as a form of hormonal contraception. However, the best results are obtained by laparoscopic treatment of the niche. A hysterectomy is also an option for women who do not wish for more children.